This POSTER has VIDEO and IMAGE elements. Hover over the image above and use the ![]() arrows to navigate
arrows to navigate
Feasibility of Implementing Brief Psychological Interventions via Telehealth in Response to COVID-19: Preliminary Retrospective Evidence from a Tertiary Orofacial Pain Clinic
Authors: Sangalli L., Fernandez Vial D., Moreno-Hay I., Boggero I.
Affiliations:
Department of Oral Health Science, Division of Orofacial Pain, University of Kentucky, College of Dentistry, Lexington, Kentucky, USA
Aim of the investigation:
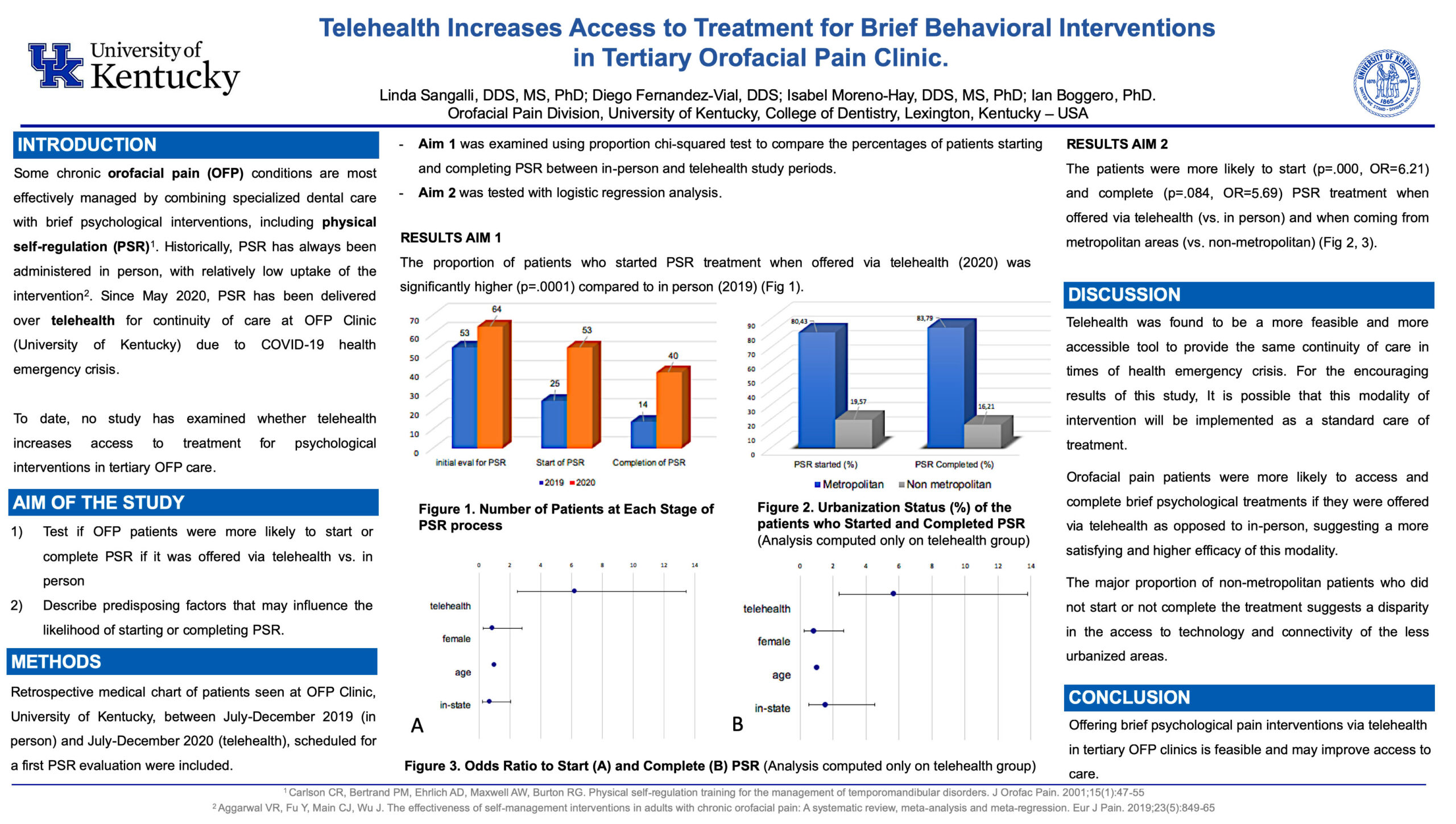
The aim of the study was to test if orofacial pain patients were more likely to start or complete a brief psychological intervention effective for managing certain chronic orofacial pain conditions (physical self-regulation, PSR), if it was offered via telehealth vs. in person. An exploratory aim was to describe demographic factors that may influence whether patients started or completed PSR via telehealth.
Methods:
Retrospective medical chart reviews were conducted of all patients seen at a large university-affiliated tertiary orofacial pain clinic between July–December 2019 (in person) and July–December 2020 (telehealth). Charts were examined for demographic information and to calculate and compare the number of patients who started and completed PSR during each study period.
Results:
Of 248 new patients seen in the clinic during the 2019 period, 53 were referred for a psychological evaluation to start PSR treatment (21.37%); of those, 25 started PSR in person (10.08%). Of 252 new patients seen during the 2020 period, 64 were referred for a psychological evaluation (25.40%); of those, 53 started PSR via telehealth (21.03%, p<.001). Patients were marginally more likely to complete all three sessions of PSR when it was offered via telehealth than in person (56.00% vs. 75.47%, p=.084). Among those who started PSR via telehealth, patients from metropolitan areas were more likely to complete the intervention than those from non-metropolitan areas (p=.045).
Conclusions:
Offering brief psychological pain interventions via telehealth in tertiary orofacial pain clinics is feasible and may improve access to care.
Acknowledgements and/or Funding Source: none



Leave A Comment